
Evolution of medical devices and clinical diagnostics present significant challenges to teams dedicated to decontamination across the globe. Decontamination methods and systems have evolved to adapt to the technological progression. Has this evolution been based upon an accurate of assessment of risk and overkill of the process?
It’s been acknowledged that certain endoscopes present a significant challenge, devices such as duodenoscopes, bronchoscopes, ureteroscopes and cystoscopes have been known to be deemed ‘high infection risk’ to patient.
The evolution of endoscopes and surgical technology is becoming more complex and often involves making devices smaller to minimize pain for patients. However, this miniaturization creates certain challenges.
Delicate devices can be difficult to clean effectively using standard decontamination processes. It’s crucial that we do not increase the risk of infection, as patient safety must remain our top priority.
Should we treat all endoscopes the same, or should we establish a hierarchy of risk based on the procedures they are used for? Should we conduct risk assessments and enhance decontamination standards for devices that access high-risk areas of the body?
Are the risks a reality? That’s an argument that is often raised. Show us the evidence? Ethically is it incorrect not to use the highest standard of decontamination possible? Spaulding has been our guidance for a generation, is it time for a rethink for decontamination procedures undertaken to reprocess higher risk devices? Based upon the Spaulding assessment, should decontamination levels of devices deemed semi-critical, be the same as for those deemed critical?
What are the issues with endoscopes and other semi critical devices? Often it is our decontamination systems, should we re-evaluate to look at ways of reducing the hazard that develops, such things as biofilms within such scopes? Do we look at drying the endoscopes and look at redeveloping the cycle configuration of the Endoscope Washer Disinfectors to counteract?
Are we investigating and testing endoscopes correctly?
Should we look to redevelop our decontamination systems in the same way we have adapted to robotic surgery? Must the device manufacturers consider the principles of decontamination and put greater emphasis on decontamination protocols?
Should we work towards sterilization of such ‘higher risk’ endoscopes and is Utopia achievable? What are the obstacles, and can we overcome or is it a culture?
Are there forgotten areas that we need to re-evaluate decontamination methods for devices deemed ‘semi-critical’ under Spaulding?
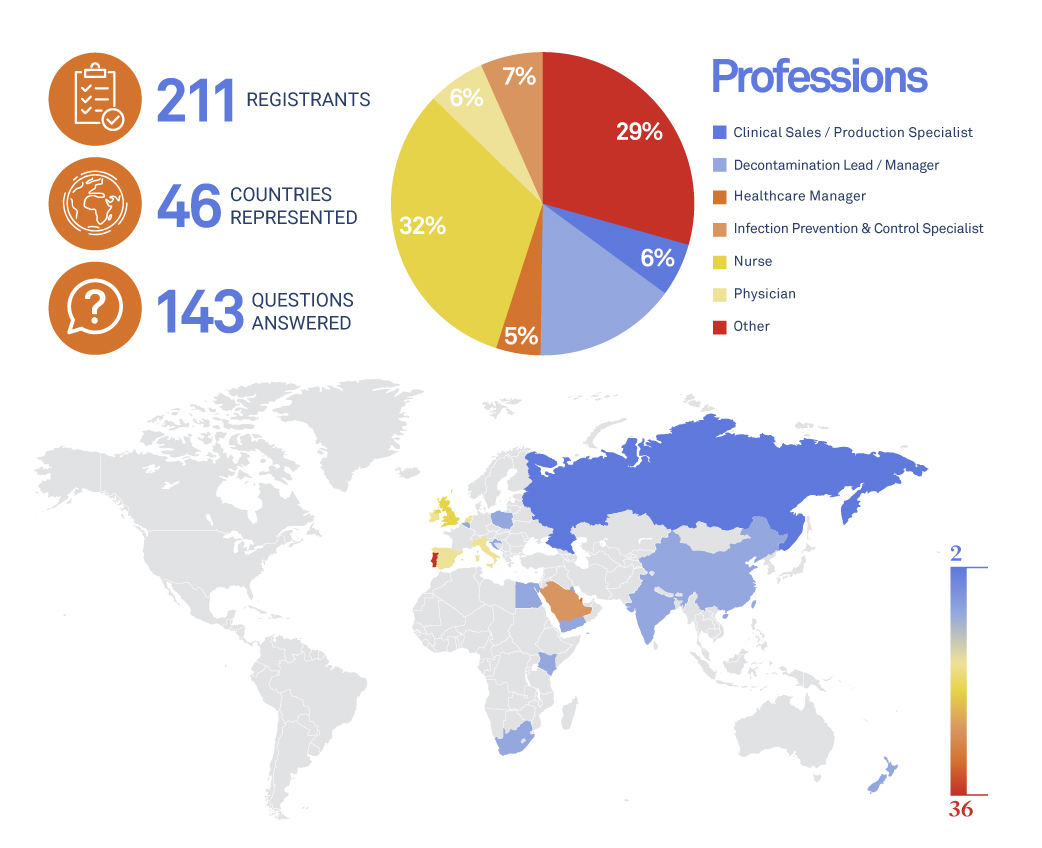
This is the Fourth webinar dedicated to “Evolution of Uro-Genital MD Reprocessing”, presented by ASP Continuous Education.
31st October 2024

John Prendergast is the Principal Decontamination Engineer working within the specialist team at NHS Wales Shared Services Partnership/Specialist Estates Services. His role is dedicated to all aspects of decontamination/reprocessing techniques of medical devices. John leads the team that provides validation services, advice and guidance to Health Boards/Trusts within Wales and works closely with Welsh governmental departments to deliver policy and strategy in this unique and often complex field. John has worked within the NHS in Wales for the past 37 years.
John is chairperson of the Central Sterilising Club and IHEEM Welsh Branch and also represents Wales on the IHEEM AE(D) Registration Board.
His participation at the event is independent of his role within NHS Wales.
- Member Institute of Healthcare Engineering and Estates Manager (UK)
- Chartered Member Institute of Decontamination Sciences (UK)
- Chairperson – Central Sterilising Club (2023 – 2026)
- Interim Chairperson – Board of AE(D) Registration – IHEEM
- IHEEM Registered AE(D)

MESSAGES
- Compliance to ISO 22441 process standard =
- Sterilizer, BI and CI, packaging manufacturers for compliance to applicable paragraphs of ISO 22441 and/or other standards
- Medical device manufacturer in partnership with sterilizer manufacturer for sterility and compatibility evaluation of medical devices
- Healthcare facility For the definition of load according to IFUs, supervision of validation, routine control, load release and maintenance of process effectiveness
- Applicable guidelines and regulation For example for use of BI , BI PCD or CI


